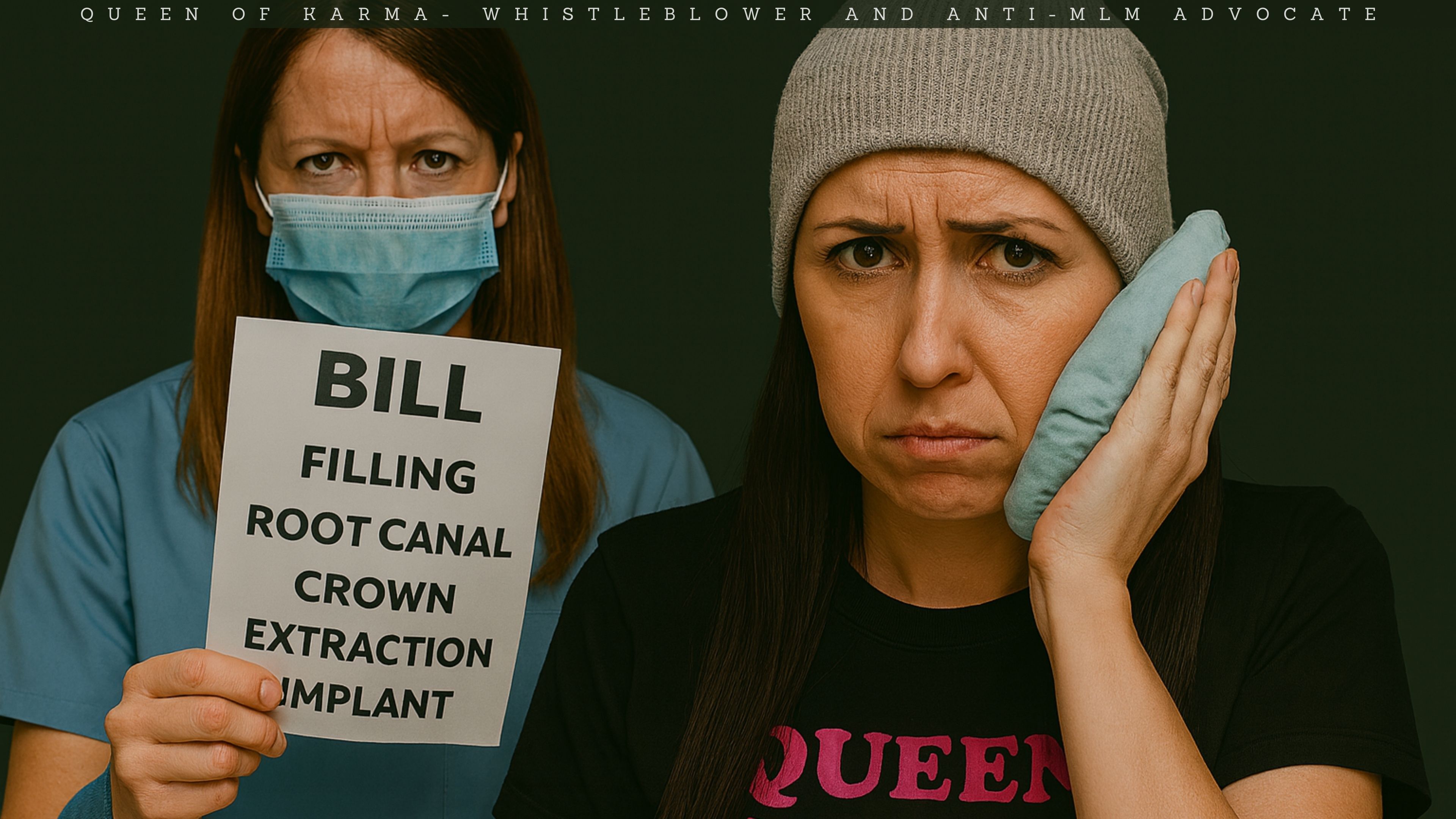
I never expected that a simple dental visit would leave me in pain, confusion and fear — or that I would spend days fighting to be heard, taken seriously, and treated safely. What happened to me wasn’t “just a bad appointment.” It was a breakdown of trust, consent, and professional responsibility. As I began to process my experience, I discovered something chilling: I am not alone.
Across Canada and the US, dental fraud, overtreatment, and unethical practices are surging — and patients are speaking out. I need to share my story and give a broader warning: dentistry has a growing accountability problem, and consumers deserve to know the truth.
What Happened to Me in That Dental Chair
I want to be completely transparent about what happened to me, because the details matter — and because this pattern is exactly how overtreatment harms patients. Here is what I experienced, step by step.
The First Filling — and a Cavity Left Behind
During the first appointment, the dentist placed a filling on a tooth that had been causing me pain. Afterward, I could still see a visible cavity — a dark, obvious spot that I was told was “just a stain.” Except that “stain” was exactly where my pain had been coming from. I pushed back. I told them something wasn’t right. I told them I believed the tooth needed a root canal. I wasn’t listened to.
I am not a dentist. I trusted the professional and figured they knew something I didn’t. I decided they knew best. When I brought it up to the dentist, I was told she could do a root canal in future, but she still denied it was a cavity and shamed me, claiming the root canal would be more for “aesthetics.”
Another Tooth Breaks — Filling Over the Nerve
Around the same time, another tooth with nerve symptoms broke further. It was a deep break, the kind that exposes or irritates the nerve. I asked if they could fix it. Instead of explaining the severity or discussing proper treatment, they:
- layered multiple layers of filling material directly over the nerve
- told me it was “deep” but “sealed well”
- reassured me it “should be fine”
- sent me home
No warning. No discussion of severe risks. No explanation of what happens when you place filling material over an already-inflamed nerve. Just “it should be fine.”
Three Days of Hell — Shock
What followed was the worst pain I’ve ever experienced. When I had my daughter, I had a c-section and I would rather have done that all over again daily than what I went through the week before Christmas this year.
For over three days, I endured:
- nerve pain so severe it sent my body into shock
- swelling
- pressure
- sleeplessness
- fear
- confusion
- a complete lack of support from the people who caused it
I went to the hospital. I was dismissed, minimized, and treated like an inconvenience. I begged the dentist to see me. They agreed to fit me in and I went in for an appointment.
The Wrong Tooth
By the time I returned to the dentist for emergency help, I had been at the hospital the entire night before. I was exhausted, terrified and in so much pain that my entire body felt like it was shutting down. The hospital had given me opiate medication, so when I walked into the dental office, I was not in a state to advocate for myself clearly — I was trying to survive the pain.
During the exam, the dentist performed the tap and cold tests again. But this time, she tapped the opposite side of the tooth — not the side where the nerve pain had been during the earlier tests. I didn’t register this in the moment. I was medicated, overwhelmed, and desperate for someone to help me. Nerve pain is unbearable.
Because of that, I agreed with her when she said the pain must be coming from the tooth beside the one that had been causing all the trouble. What I didn’t take into account — and what she didn’t seem to consider — was that:
- all nerves in the front teeth are interconnected
- the entire front of my mouth was swollen and hypersensitive
- my chin felt bruised and tender
- my front teeth have two nerves, which is rare but something the dentist should have identified immediately.
When a tooth with two nerves is inflamed, it can easily make surrounding teeth feel like they’re in crisis too. That sensitivity wasn’t a sign that the neighboring tooth needed a root canal, it was a sign that the original problem tooth was radiating pain through the entire area.
But in the middle of all this — swollen, medicated, and in agony — I trusted her judgment. After all, she is the dentist. I am just the consumer protection advocate. What do I know about teeth?
She assured me that the tooth beside the problem tooth needed a root canal. Then she performed a root canal on that tooth. This happened days into the ordeal, right in the middle of the worst swelling, the worst nerve pain, and the worst confusion.
Looking back, it’s clear that the wrong tooth was treated — not because I misled anyone, but because I was in no condition to challenge what I was being told, and because the dentist didn’t take the time to reassess the situation carefully.
The Pain Didn’t Stop
After the root canal was done on the wrong tooth, I expected — like any reasonable patient — that the pain would begin to ease once the freezing wore off. Even with complications, most people feel some improvement within 24 hours.
But when the numbness faded, the reality hit me like a freight train. I was still in severe, unrelenting pain — the kind that makes your whole body shake, the kind that steals your sleep, the kind that tells you something is deeply, dangerously wrong.
And this was more than a day after the procedure. That was the moment I knew: the real problem tooth had never been treated.
I had a follow-up appointment scheduled for Christmas Eve, but that was still over three days away, and I was in no condition to wait. I went back to the dentist twice, desperate for help, explaining that the pain was unbearable and something was clearly wrong.
Both times, I was refused. I was told to wait until my appointment. I was told to “give it time.” I was dismissed, again. Meanwhile, the pain was escalating, not improving.
With nowhere else to turn, I ended up back at the hospital — twice. I was exhausted, terrified, and still dealing with the aftermath of nerve pain that had already pushed my body into shock earlier in the week. I kept explaining that something was wrong with my tooth, that the pain wasn’t normal, that I couldn’t wait days for help.
But I still couldn’t get relief. I still couldn’t get answers. I still couldn’t get anyone to treat the actual problem. At one point, the doctor in the Emergency Room asked me “What do you want us to do for you?” and I thought, “If the doctor cannot help my body out of pain and shock, nobody can.”
The hospital gave me more opiates and an Ativan, asked me not to scream out in pain because it would “scare the other patients,” and treated me like I was a burden. At one point, I told them my body was in shock and I was starting to see double and felt extremely weak and the nurse told me to follow her to a room then walked so fast, I couldn’t keep up. I asked if I could get some help and they told me to “just keep walking.” I felt hopeless. I went home from my third hospital visit wondering if I had three more days of this shock and pain. Then I wondered how I would get through it and how long it would take for my body to come back down. Would I be well enough for Christmas?
It was Sunday night and I was out of options. The good news was that the next morning, I might find a dentist office that would take me.
Begging for Help from Dentist to Dentist
At this point, I was running out of options.
It was the holidays. Clinics were closed. My own dentist refused to see me. The ER doctor wanted ME to diagnose my own problem and tell them how to treat it. And I was in agony. So I did what no patient should ever have to do: I went from dentist to dentist, begging someone — anyone — to take me. I walked up and down one of the main roads, from clinic to clinic, asking every receptionist the same desperate question: “Can you take an emergency right now?”
Most were closed. Some weren’t accepting emergencies. Some simply couldn’t fit me in. And then there was the insurance barrier — something I never expected to face in the middle of a medical crisis. Several offices told me they couldn’t take a new X-ray because there was a chance the Canadian Dental Care Plan wouldn’t cover it. Without that X-ray, they couldn’t legally or ethically treat me. And the only way around it was to have my existing X-rays faxed over from the very dentist who had put me in this situation in the first place.
I was trapped in a bureaucratic loop while my face throbbed, my nerves screamed, and the clock ticked toward Christmas.
Finally, I found a dentist who agreed to see me. She offered to fit me in upon closing. The receptionist even offered to tell my last clinic to fax over my X-rays. It was a Christmas miracle!
I returned later in the day. Within minutes of examining me, they saw the issue immediately. They identified the real problem tooth. They recognized the unusual nerve anatomy — the two-nerve structure in my front tooth that the previous dentist had missed entirely. They understood why the pain had been radiating through my entire face. And they treated the correct tooth. Extracted it, immediately.
The relief was immediate and profound — not because the pain vanished instantly, but because someone finally listened, understood, and acted.
This Should Never Have Happened
No patient should have to:
- endure days of untreated nerve pain
- be dismissed by their own dentist
- be refused emergency care
- go to the hospital multiple times
- wander from clinic to clinic during the holidays
- beg for someone to take their pain seriously
- receive a root canal on the wrong tooth
- rely on another dentist to fix what their own clinic ignored
But this is exactly what overtreatment and mismanagement look like in real life. It’s not just about money. It’s about harm. It’s about trauma. It’s about patients being left to suffer because the system protects providers, not the people they’re supposed to care for.
The Hidden Business Model: Overtreatment
Overtreatment is one of the most profitable — and least regulated — forms of dental misconduct. It happens when a dentist performs unnecessary procedures, or performs multiple procedures on the same tooth, not because the patient needs them, but because each step generates a new billable code.
Here’s how the pattern typically unfolds, and how it mirrors what happened to me.
Step 1: The Filling That Was Never Going To Work
In legitimate dentistry, a filling is used when:
- the cavity is small
- the nerve is healthy
- the tooth structure is stable
But when a tooth is already showing signs of nerve involvement — deep pain, swelling, temperature sensitivity, or radiographic evidence — dentists are not supposed to “try a filling and see.”
Why?
Because they already know the filling will fail.
Yet some clinics do it anyway because:
- A filling is billable
- It looks like “conservative care”
- It delays the real treatment
- It sets up the next, more expensive procedure
This is the first layer of the scam.
Step 2: The Predictable Failure — “Needing” a Root Canal
Once the filling inevitably fails (because the nerve was compromised the whole time), the dentist can now say:
“Looks like the tooth needs a root canal after all.”
This creates a second billable event:
- diagnostic imaging
- the root canal itself
- the buildup
- the crown
All on the same tooth.
In many fraud cases, investigators found that dentists intentionally placed fillings on teeth that clearly needed root canals, because it allowed them to bill twice.
This is exactly the pattern I experienced — twice.
Step 3: If the Root Canal Fails, They Profit Again
Root canals can fail for many reasons, but in overtreatment cases, failure is often predictable because:
- the tooth was already too compromised
- the initial filling delayed proper treatment
- the infection worsened during the delay
- the tooth structure was weakened
When the root canal fails, the next step is:
- extraction
- implant
- bridge
- or denture work
Each one is another billable procedure. This means a single tooth can generate:
- a filling
- a root canal
- a crown
- an extraction
- and possibly implant work
Five separate billing opportunities — all from one tooth that should have been treated correctly the first time.
Overtreatment isn’t always dramatic. It often looks like:
- “Let’s try this first.”
- “We’ll see how it goes.”
- “It might work, but no guarantees.”
But when a dentist already knows the tooth needs a root canal, offering a filling first is not “conservative.” It’s profitable. Ethical dentists don’t gamble with your pain. They don’t “try” procedures they know won’t work. They don’t set you up for multiple billable failures.
In my case:
- Two teeth were treated with fillings even though the symptoms pointed to nerve involvement.
- Both fillings failed.
- Both teeth escalated to severe pain and swelling.
- I ended up in the hospital.
- I was dismissed and minimized when I sought help.
This is not normal dentistry. This is not “bad luck.” This is a pattern — one that matches the overtreatment schemes currently being exposed across Canada and the US.
Why Patients Don’t Realize It’s a Scam
Many patients won’t even realize they are being scammed in the moment. This is because the process is disguised as:
- “trying the least invasive option”
- “saving you money”
- “being cautious”
- “avoiding unnecessary root canals”
But in reality, it’s the opposite:
- it costs more
- it causes more pain
- it delays proper treatment
- it increases the risk of complications
- it maximizes billing
Patients trust their dentists. Scammers exploit that trust. Most people don’t walk into a dental office thinking:
- “Is this person scamming me?”
- “Are they overtreating me?”
- “Are they billing insurance fraudulently?”
We assume ethics. We assume professionalism. We assume they’re following standards of care. But the reality is:
- some clinics prioritize profit over patients
- some dentists cut corners
- some push unnecessary procedures
- some ignore symptoms to protect themselves
- some dismiss patients to avoid accountability
Trust can become a blind spot and unethical providers exploit that blind spot ruthlessly.
Dentistry: A Systemic Issue
Dentistry is often treated as a medical profession — but it is not regulated like one. Across Canada, the US and New Zealand, dentistry operates in a fragmented, inconsistent, and often opaque regulatory environment. Patients assume dentists are held to the same standards as physicians. But the reality is far more complicated — and far less protective.
There is:
- no universal oversight
- no standardized second-opinion requirement
- no real-time auditing
- limited transparency
- weak complaint systems
- minimal accountability
Patients assume someone is watching. Someone is checking. Someone is making sure dentists follow the rules. But in reality, most oversight is reactive — not proactive. By the time a patient realizes something is wrong, they’re already in pain, already traumatized, and already financially exploited. By the time a dentist is caught, the damage is already done.
Canada: A Patchwork of Provincial Regulators
In Canada, dentistry is regulated province by province, not nationally. Each province has its own dental regulatory authority, and while they collaborate through the Canadian Dental Regulatory Authorities Federation (CDRAF), there is no unified national oversight system.
This means:
- standards vary by province
- complaint processes vary
- disciplinary transparency varies
- enforcement varies
- patients have no national body to escalate concerns to
Even the Canadian Dental Association (CDA) is not a regulator — it is a professional association representing dentists, not patients.
The new Canadian Dental Care Plan (CDCP) is a major federal initiative, but it does not regulate dentists. It is an insurance program, not an oversight body. It will pay dentists — but it will not police them.
This means:
- dentists will still self-regulate
- provincial colleges will still handle complaints
- there is still no national patient-protection system
- overtreatment and billing abuse remain possible
The CDCP may increase access to care, but it does not fix the underlying regulatory gaps. In fact, some may argue it opens up a new vulnerable population for dentists to scam.
United States: A Market-Driven Industry
In the US, dentistry is regulated at the state level, and the American Dental Association (ADA) actively advocates to minimize federal regulation on dental practices.
This means:
- no national oversight
- no standardized patient-protection system
- no unified complaint process
- no national auditing of dental billing
- no federal requirement for second opinions
The ADA’s Own Advocacy materials emphasize reducing regulatory burden on dentists, not increasing accountability or transparency for patients.
In a market-driven system, dentistry often behaves like a private business first and a healthcare service second. This creates fertile ground for:
- overtreatment
- unnecessary procedures
- insurance fraud
- aggressive upselling
- corporate dental chains prioritizing profit
Patients assume the system protects them but the system is designed to protect providers and doesn’t want to change anytime soon.
New Zealand: Small Country, Large Oversight Gaps
New Zealand’s dental system is regulated by the Dental Council of New Zealand, but like Canada and the US, it is self-regulating and reactive, not proactive.
While NZ has stronger public health structures that the US, dentistry still suffers from:
- limited real-time auditing
- slow complaint processes
- minimal transparency around disciplinary actions
- no national second-opinion requirements
- no independent patient-advocacy body
New Zealand also faces workforce shortages, which has led to Discussions About Loosening Regulations for foreign-trained-dentists — raising concerns about patient safety and oversight.
A Global Pattern: Dentistry as a Trade, Not a Medical Discipline
Across all three countries, the same systemic issues appear:
- Self-Regulation
Dentists regulate themselves through professional colleges or boards. This creates inherent conflicts of interest. - No National Oversight
Canada and the US rely on provincial/state regulators. NZ has a single regulator, but it is still self-governing. - Weak Complaint Systems
Complaints are slow, opaque, and often resolved internally. - No Real-Time Auditing
Unlike hospitals or pharmacies, dental clinics are rarely audited unless a complaint is filed. - No Standardized Second Opinions
Patients are not required or encouraged to seek second opinions before major procedures. In fact, in many cases, patients cannot do this. Many insurance companies have financial caps on the amount of treatments or X-rays a patient can be provided. So a second opinion would have to be paid for out-of-pocket which most patients cannot afford. - Limited Transparency
Disciplinary actions are often hidden, sealed, or difficult for the public to access. - Market Forces Drive Treatment
In all three countries, dentistry is largely privatized. Profit incentives shape treatment decisions.
Dentistry Needs Oversight NOW
We are living through a moment of reckoning in dentistry — and it’s being driven not by regulators, not by professional associations, but by patients. Ordinary people, harmed by unethical or unqualified providers, are turning to social media to expose what regulators have failed to prevent. And the stories coming out are shocking.
The Fake Veneer Techs Targeting Vulnerable Patients
Across TikTok and Instagram, unlicensed “veneer techs” are advertising cheap cosmetic dentistry — often at half the price of legitimate clinics. These individuals have no dental training, no certification, and no oversight. They operate out of strip malls, private homes, and makeshift studios.
Dentists and journalists have warned that these procedures can cause irreversible harm, including damaged enamel, infections, and long-term complications.
One high-profile case involved a TikTok Creator who was arrested after allegedly scamming patients with fake veneers and damaging their teeth and gums.
This is happening because there is no meaningful enforcement preventing unlicensed individuals from performing dental procedures and because desperate patients are being priced out of legitimate care.
Cheap Braces From TikTok Anyone?
Another viral case involved a woman on TikTok offering braces for just $150 — a fraction of what legitimate orthodontic treatment costs. She wasn’t a licensed orthodontist. She wasn’t even a licensed dental professional. In fact, she also sold wigs and could do your eyelash extensions.
Yet she was applying brackets and wires in non-clinical settings, often to teenagers and young adults who believed they were getting a deal. This wasn’t orthodontics. This wasn’t safe. This was unregulated dental work being performed by someone with no qualifications. Well, maybe she had the qualifications to do your lashes…
The news of her services spread like wildfire because:
- people are desperate for affordable dental care
- social media makes scams look polished and legitimate
- there is no centralized oversight preventing unlicensed individuals from offering dental procedures
- regulators typically act only after harm occurs
The $150 price tag wasn’t generosity — it was bait. The reason it worked is because the dental system is failing people so badly that even dangerous alternatives look appealing.
Patients Speaking Out Because Regulators Aren’t Protecting Them
More and more people are turning to TikTok, Instagram, YouTube, and Reddit to expose:
- overtreatment
- unnecessary root canals
- fraudulent billing
- unlicensed cosmetic dentistry
- botched veneers
- corporate dental chains upselling vulnerable patients
- dentists who ignore pain, dismiss symptoms, or refuse follow-up care
Social media has become the only place where patients feel heard. That alone is an indictment of the system. When people have to go viral to get justice, something is deeply wrong.
Why I’m Speaking Out
I’m not accusing anyone of a crime — that’s for regulators and investigators. But I am naming a pattern that harmed me and is harming others.
My experience fits the exact structure of Overtreatment Cases currently being prosecuted and reported in the News. And if it happened to me, it’s happening to others — quietly, invisibly, and without accountability.
People deserve to know what overtreatment looks like so they can protect themselves. But this isn’t just about my story. It’s about a system that allows these stories to happen in the first place.
For too long, dentistry has operated in a regulatory vacuum — a patchwork of provincial, state, and national rules that prioritize providers over patients. Across Canada, the US, and New Zealand, oversight is inconsistent, complaints are slow, disciplinary actions are often hidden, and real-time auditing is almost nonexistent. Dentistry is treated like a private business, not a medical discipline, and patients pay the price.
And now we’re seeing the consequences everywhere.
Fake veneer clinics run by unlicensed “techs.”
TikTok creators offering $150 braces in living rooms.
Corporate dental chains upselling vulnerable patients.
People being pushed into unnecessary root canals, crowns, and extractions.
Patients discovering too late that they were mislead, dismissed, or outright harmed.
These aren’t isolated incidents — they’re symptoms of a broken system.
What’s different now is that patients are finally speaking out. They’re turning to TikTok, Instagram, YouTube, and Reddit because regulators aren’t protecting them. Social media has become the only place where people feel heard, believed, and validated. And the stories being shared are exposing a truth that the dental industry has avoided for decades:
Without real oversight, dentistry becomes a breeding ground for overtreatment, fraud, and preventable harm.
That’s why I’m speaking out.
Because silence protects unethical practices.
Because shame protects scammers.
Because sunlight protects patients.
I’m sharing my story so others can recognize the red flags I didn’t know to look for. I’m sharing it because people deserve transparency, honesty, and ethical care. I’m sharing it because the rise of dental scams and patient-led exposés shows that we are at a turning point — and we cannot afford to look away.
If we want change, we have to demand it. We need national oversight, real-time auditing, transparent disciplinary records, protections against overtreatment, and laws that prevent unlicensed individuals from performing dental procedures. We need systems that protect patients, not providers.
I’m speaking out because no one should have to go through what I went through. Because the only way to fix a broken system is to name the harm, expose the patterns, and refuse to stay silent. This is our moment and I refuse to waste it.
I’m writing this article because when I went to my first dental appointment, she asked me what I do for work and I said “I expose scams. I am a consumer protection advocate.” Which is hilarious because if you’re going to run a dental scam, maybe don’t pick the woman who studies fraud the way other people watch Netflix.
By Beth Gibbons (Queen of Karma)
Beth Gibbons, known publicly as Queen of Karma, is a whistleblower and anti-MLM advocate who shares her personal experiences of being manipulated and financially harmed by multi-level marketing schemes. She writes and speaks candidly about the emotional and psychological toll these so-called “business opportunities” take on vulnerable individuals, especially women. Beth positions herself as a survivor-turned-activist, exposing MLMs as commercial cults and highlighting the cult-like tactics used to recruit, control, and silence members.
She has contributed blogs and participated in video interviews under the name Queen of Karma, often blending personal storytelling with direct confrontation of scammy business models. Her work aligns closely with scam awareness efforts, and she’s part of a growing community of voices pushing back against MLM exploitation, gaslighting, and financial abuse.





Holy hell, what an ordeal. I bet you didn’t think you would end up advocating for something quite different from the usual, but ultimately there are so many dodgy, scammy, unscrupulous and harmful things going on. They don’t know who they messed with.